How to Ask Your Doctor for a GLP-1 Prescription: 6 Steps to Speak Up and Get Heard
Author
glp winnerDate Published
- Twitter
- Facebook
- LinkedIn
- Instagram
- Copy Link
GLP-1 medications like Wegovy® (semaglutide) and Zepbound™ (tirzepatide) are changing the way people manage weight, diabetes, and even heart health. But let’s be real: getting a prescription isn’t always simple. Some doctors aren’t familiar, some don’t want to deal with prior authorizations, and others just say “try harder” when you’ve already tried everything.
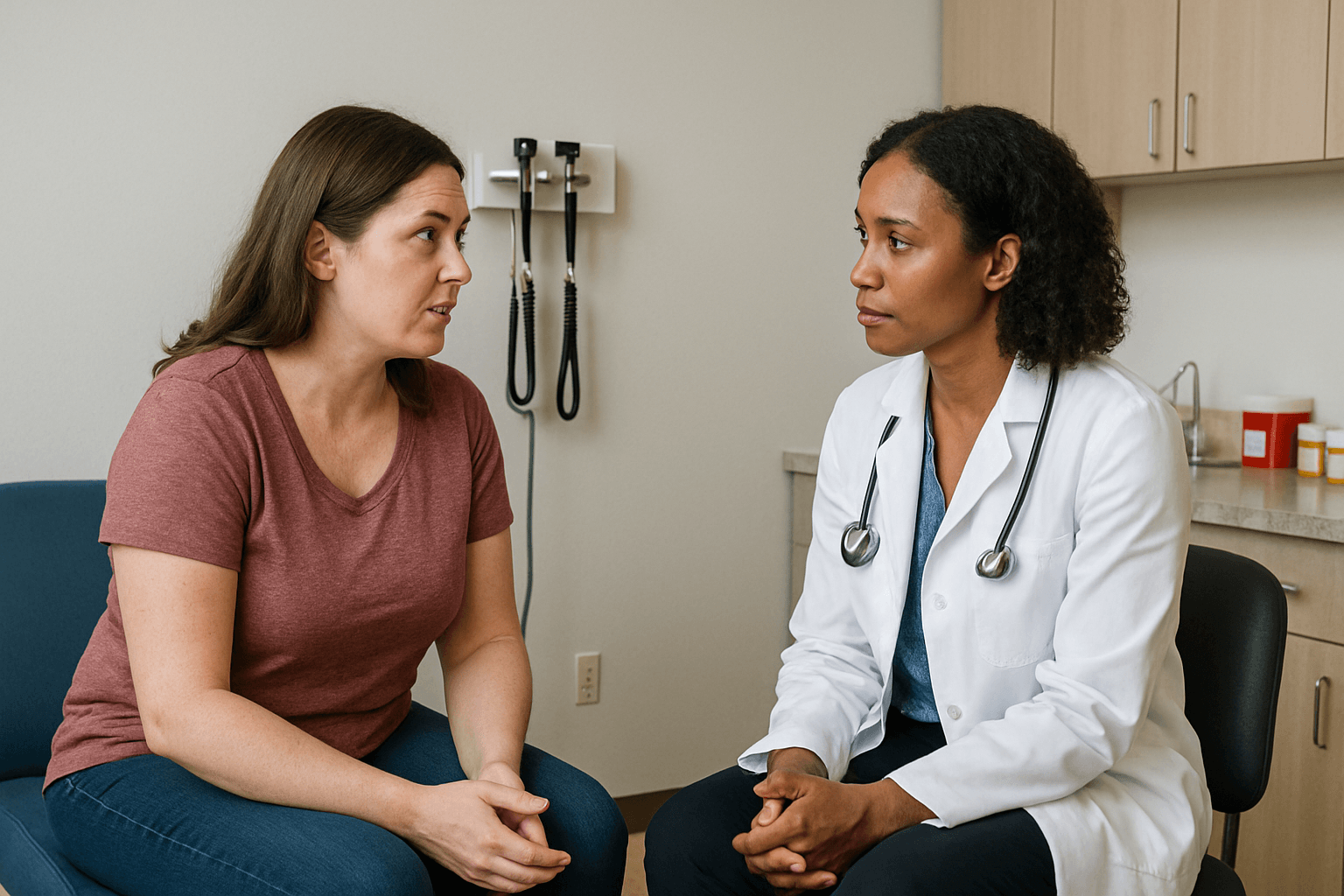
That’s where self-advocacy comes in. Speaking up for yourself in healthcare isn’t being “difficult.” It’s protecting your health. UCLA’s LEND program calls self-advocacy “a key part of better health and fair treatment” (UCLA LEND).
This guide takes six practical tips from Sabina Hemmi (GLP Winner co-founder) and turns them into an action list. Think of it as your playbook for asking a doctor about GLP-1 therapy with confidence.
1. Bring a Friend Who Will Back You Up
Doctor visits can be nerve-wracking. Having someone with you changes the whole vibe.
Choose a friend or family member who’s not afraid to speak up. If you’ve got one “too nice” friend and one who’s blunt, bring the blunt one. They don’t need to take over, but they can make sure you don’t shrink back if the doctor gets dismissive.
And yeah, sometimes just having another body in the room helps you feel braver. Studies even show that patients with advocates by their side report feeling more confident in their decisions (NIH).
2. Take Notes by Hand — Stay Present
Skip the phone. It can look like you’re distracted or Googling mid-conversation. Bring a notebook and a pen.
Write your main question at the top (something like: “Can GLP-1 therapy help me with my weight and overall health?”). Then, when the doctor talks, jot notes in your own words.
Here’s the trick: after you ask a question, stop. Be quiet. Let the silence work for you. It gives the doctor space to actually answer instead of rushing past your concern.
3. Bring a Written History of What You’ve Already Tried
Many doctors fall back on: “Try diet and exercise for six months, then come back.”
You can save time by showing you’ve already put in that work. Write a short timeline of your efforts:
- High school: calorie counting → results
- College: keto for 2 years → lost some, gained it back
- Last year: gym 4x a week → weight barely moved
This proves you’re serious and stops the “try harder” loop before it starts. The Obesity Action Coalition has written about weight bias in healthcare, and documenting your history is one way to push back (Obesity Action Coalition).

Letting your provider know about any regular activities you attend to increase your physical activity helps to show you have a long-term dedication to losing weight on your own.
4. Talk About Health Beyond Weight
Doctors think in terms of long-term outcomes. Yes, weight matters, but GLP-1s are about more than the number on a scale.
In clinical studies, FDA-approved medications like Wegovy® were shown to reduce the risk of major heart problems by around 20% (FDA). They also improve blood sugar control in type 2 diabetes.
So, frame your goals like this:
- “I want to reduce my risk of diabetes or heart disease.”
- “I want more energy to be active with my kids.”
- “I want to stay healthier as I age, not just lose pounds.”
That language helps doctors see you’re focused on health, not just “beach body” goals.
5. Set Realistic, Long-Term Goals
Crash expectations turn doctors off. If you say, “I want to look different by next month,” they’ll tune out.
Better: think about one year from now. In studies of FDA-approved GLP-1s, patients lost 10–20% of their weight over 12–18 months (Cleveland Clinic). That’s steady, sustainable progress.
Try saying:
- “If I lost 15% of my weight in a year, how would that help my health risks?”
That shows you’re realistic and thinking long-term.
6. Show You’ve Checked Coverage and Cost
Doctors don’t want to prescribe something you can’t afford to fill. It feels like wasted effort.
Do the homework first:
- Call your insurance to see if GLP-1s are covered for weight loss.
- Check manufacturer coupons on brand websites
- Use GLP Winner’s cost tool to get estimates with or without insurance. See here for Wegovy, Zepbound, Mounjaro, and Ozempic cost estimates on GLP Winner.
This tells your doctor you’re serious — and takes away a common reason for them to say “no.”

A lot of this can be done from your own home, so you can take your time with the research and educating yourself to make sure you're weighing your options.
What If Brand Medications Aren’t an Option?
Here’s the hard truth: not everyone will get access to brand-name GLP-1s, even if you do everything right. Sometimes FDA approved medication is not a good fit for you.
That doesn’t mean your journey ends. Some providers prescribe compounded GLP-1 medications through compounding pharmacies.
Here’s what you should know:
- Compounded GLP-1s are not FDA-approved. That means the FDA has not reviewed them for safety or effectiveness.
- Compounding pharmacies themselves are state licensed pharmacies, but the drugs aren’t the same as FDA-approved products like Wegovy® or Zepbound™.
- For some patients, compounded versions are the only accessible path because they have a medical need for customized medication.
At GLP Winner, many providers in our network do prescribe compounded medications when brand versions aren’t an option. We’re transparent about the difference so you can make the choice that’s right for you.
Bonus: Accept If This Isn’t the Right Doctor
Even with all your prep, some doctors won’t prescribe GLP-1s. Sometimes it’s about time, prior authorization paperwork, or limitations on their practice. Some doctors even have a bias against the medication.
That’s okay. You can:
- Ask for a referral to an endocrinologist or obesity medicine doctor.
- Use GLP Winner to find providers who do prescribe GLP-1s, including compounded options when needed.
Remember: one “no” isn’t the end. It might mean you haven’t found the right partner yet. If your doctor says you’re not a good fit for GLP-1s be sure to ask why and listen to their reasoning. Not every person should take these medications. It depends on your individual medical situation.
Wrap-Up: Your Health, Your Voice
Self-advocacy isn’t about being pushy. It’s about showing up with your history, your goals, and your homework in hand. And honestly, yeah, it can feel awkward to pull out a notes in front of your doctor. But it works. Doctors respect patients who come prepared.
If the first provider doesn’t listen, you have other options — and we’re here to help you explore them.
FAQs: GLP-1 Prescriptions and Self-Advocacy
Q: What is a GLP-1 medication?
A: GLP-1 receptor agonists are prescription drugs that help regulate blood sugar, slow digestion, and reduce appetite. Some FDA-approved versions (like Wegovy® or Zepbound™) are used for weight management and Ozempic and Mounjaro are FDA approved for type 2 diabetes.
Q: Are compounded GLP-1s the same as brand medications?
A: No. Compounded GLP-1s are not FDA-approved. That means they haven’t gone through the same safety and effectiveness review as branded drugs. Some providers prescribe them when brand-name medications aren’t an option, but they are not the same as Wegovy® or Zepbound™.
Q: How much weight can I lose on a GLP-1?
A: In clinical studies of FDA-approved GLP-1s, patients lost about 10–20% of their weight over 12–18 months (NEJM). Everyone’s results vary, and side effects are possible, which is why close medical follow-up is important.
Q: What if my doctor doesn’t like to prescribe GLP-1s?
A: You still have options. You can ask for a referral to an obesity medicine specialist or endocrinologist. You can also use tools like GLP Winner to find providers who are familiar with GLP-1 care, including those who may prescribe compounded versions when brand drugs aren’t available.
Sources
Keep Reading
We’ve all been hearing about the shortage of tirzepatide or semaglutide, but what is a shortage? How does it impact compounding?

FDA: “many of the adverse events reported for compounded versions appear to be consistent with adverse events for the FDA‑approved products.”

It's the end of the shortage style compounding with essential copies. Now compounding requires a medical justification.
