Top Misconceptions About GLP-1s (Debunked)
Author
glp winnerDate Published
- Twitter
- Facebook
- LinkedIn
- Instagram
- Copy Link

GLP-1 medications like Wegovy® (semaglutide) and Zepbound® (tirzepatide) are everywhere right now. You see them in news stories, in celebrity interviews, on TikTok, and maybe even whispered about at your local gym. With that much buzz, myths spread fast. Some are based on small truths, some are pure clickbait, and some are just flat-out wrong.
This post breaks down the biggest misconceptions people keep repeating about GLP-1s, with the facts to set the record straight.
Misconception 1: GLP-1s are just “diet pills”
When people call these meds “diet pills,” they’re usually picturing something cheap and quick that makes weight fall off. That’s not what GLP-1s are.
They’re prescription medications that mimic a natural hormone in your body called glucagon-like peptide-1. This hormone helps your pancreas release insulin when blood sugar is high, and it also tells your brain when you’re full. So they’re working on blood sugar and appetite at the same time.
In clinical trials, people taking FDA-approved GLP-1s lost about 10–20% of their body weight over 12–18 months when combined with diet and exercise (NEJM). That’s a world apart from a “quick fix” pill.
Misconception 2: They work overnight
You won’t take one shot and wake up thin. Doctors start patients on a low dose and increase it slowly to help with side effects. That means results take time.
Most people don’t notice real changes until they’ve been on the medication for a few months. It’s a slow, steady process—that’s what makes the results more sustainable (FDA).
Misconception 3: Once you hit your goal weight, you can just stop
It would be nice if GLP-1s “locked in” your results forever. But for most people, that’s not the case. In studies, people who stopped semaglutide regained about two-thirds of the weight they lost within a year (STEP 1 extension study).
That doesn’t mean no one can come off the medication. Some research suggests that tapering slowly, while sticking to nutrition, exercise, and coaching, helps people keep more of the weight off (Pharmacist.com). But others may need to stay on GLP-1s long term to maintain results.
So the real answer is: stopping is possible, but it takes planning, and it doesn’t work for everyone.
Misconception 4: They’re just for celebrities
Celebrities might talk about them, but the FDA approved these medications for very specific groups: people with obesity (BMI 30 or higher) or people who are overweight (BMI 27 or higher) with health problems like type 2 diabetes or high blood pressure (FDA prescribing info).
The real barrier is cost and insurance coverage, not fame. Some people turn to compounded GLP-1s, but it’s important to know these versions are not FDA-approved, and their safety and effectiveness aren’t guaranteed.
Misconception 5: You don’t need healthy habits anymore
That’s a romantic idea, but the data say otherwise. People who pair GLP-1s with good nutrition and exercise tend to get better results. In one clinical trial, combining exercise + liraglutide helped with lasting weight loss more than either method by itself (NEJM).
A nutrition-medicine consensus also recommends diet therapy, protein balance, micronutrient support, and movement as essential “boosters” for GLP-1s (ASN).
So yes — the meds do heavy lifting, but the habits help make it stick.
Misconception 6: The side effects hit everyone and are always severe
This one gets repeated a lot, but it’s exaggerated. It’s true that GLP-1s can cause side effects—most often nausea, constipation, or diarrhea. But not everyone gets them, and for many people they’re mild and fade over time.
Doctors start patients at very low doses and raise them slowly to help minimize side effects. In clinical trials, most people were able to stay on the medication, which shows that while side effects are common, they’re usually not deal-breakers (Cleveland Clinic).
There are also more rare but serious risks, like gallbladder problems or thyroid concerns. The thyroid risk comes from animal studies, where rodents given very high doses developed thyroid C-cell tumors (Bioscientifica). This hasn’t been proven in humans, but doctors take it seriously enough that people with certain thyroid cancers usually won’t be prescribed GLP-1s.
So yes, side effects are part of the picture—but the idea that everyone will feel awful on GLP-1s just isn’t true.
Misconception 7: GLP-1s cause blindness
This myth has been all over the news. Blindness is not a known or proven side effect, but there are some studies looking at possible eye risks.
A recent study in JAMA Ophthalmology and coverage from the American Optometric Association noted a possible link between GLP-1 use and non-arteritic anterior ischemic optic neuropathy (NAION), a condition that affects the optic nerve. People with diabetes are already at higher risk for vision issues, and quick changes in blood sugar may sometimes make eye conditions worse. The European Medicine Association also decided to update product information with the warning that NAION is a very rare side effect possible for those taking semaglutide medications (EMA).
The safest approach? If you’re on a GLP-1, get regular eye exams and if you have any sudden changes, like vision loss, shadows, or other issues, go to the ER in case of urgent issues.
Misconception 8: Everyone gets “Ozempic face”
“Ozempic face” became a viral phrase online to describe how some people’s faces look thinner or older after losing weight on GLP-1s. It’s not the drug targeting your face—it’s what happens when fat under the skin is lost quickly, which can happen with any form of rapid weight loss.
Not everyone gets it, and for many it’s less noticeable. Doctors recommend aiming for slower, steadier weight loss and keeping a balanced diet with enough protein and nutrients. That helps protect both skin and muscle health (Journal of Clinical Medicine).
Why do these myths spread so fast?
Because “GLP-1s cause blindness” makes a way better headline than “some early studies suggest there may be risks for certain patients.” Social media loves drama, not nuance. Add in celebrity talk, patchy insurance coverage, and new studies dropping every few months, and rumors spread fast.
That’s why it’s better to double-check with trusted sources like the FDA, Cleveland Clinic, or UCLA Health when you’re looking for facts (not your neighbors).
What to ask your doctor
If you’re curious about GLP-1s, here are a few smart questions to bring up:
- Am I eligible for an FDA-approved GLP-1?
- What side effects should I expect, and how can I manage them?
- How fast should I expect to lose weight?
- What’s the plan if I stop taking the medication?
- How often should I check in with you?
- If insurance doesn’t cover it, what safe alternatives exist?
FAQs
Are GLP-1s just diet pills?
No. GLP-1s are FDA-approved prescription medications that mimic a natural hormone to regulate blood sugar and appetite. They’re very different from over-the-counter “diet pills.”
Do GLP-1s work instantly?
No. Doctors usually start with a low dose and raise it slowly. It often takes a few months before people notice steady results.
Will I keep the weight off if I stop taking GLP-1s?
Not always. Many people regain weight after stopping. That’s why doctors recommend a long-term plan for weight management.
Do side effects hit everyone who takes GLP-1s?
No. Side effects like nausea or constipation are common but don’t affect everyone. For most, they’re mild and improve over time. Serious side effects are rare but possible, which is why medical follow-up is important.
Can GLP-1s make you go blind?
Blindness is not a proven side effect. Some studies suggest a possible link to rare eye conditions, but more research is needed. Regular eye exams are recommended, especially for people with diabetes.
Does everyone get “Ozempic face”?
No. “Ozempic face” is a social media term for facial changes after rapid weight loss. It doesn’t happen to everyone, and slower, steady weight loss with a balanced diet may help reduce the risk.
Bottom line
GLP-1s are powerful medications, but they’re not magic. They don’t work instantly, they don’t work without lifestyle support, and they don’t come without side effects. But the extreme myths—like “they’ll make you blind” or “everyone gets Ozempic face”—don’t tell the full story either.
The reality is more balanced: for many people, GLP-1s can be life-changing when used safely, under the guidance of a doctor. Myths will keep swirling, but facts and follow-up care matter more than viral soundbites.
Sources
Keep Reading
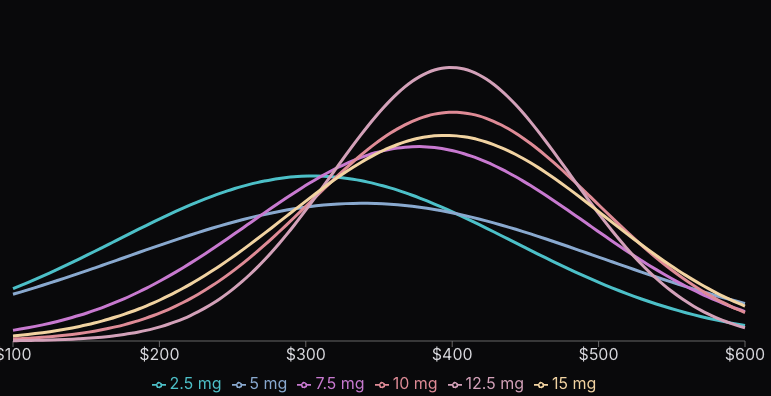
We put together some data on prices for compounding. Most of the data is from self reported prices from over 6,000 people we’ve polled.
We’ve all been hearing about the shortage of tirzepatide or semaglutide, but what is a shortage? How does it impact compounding?
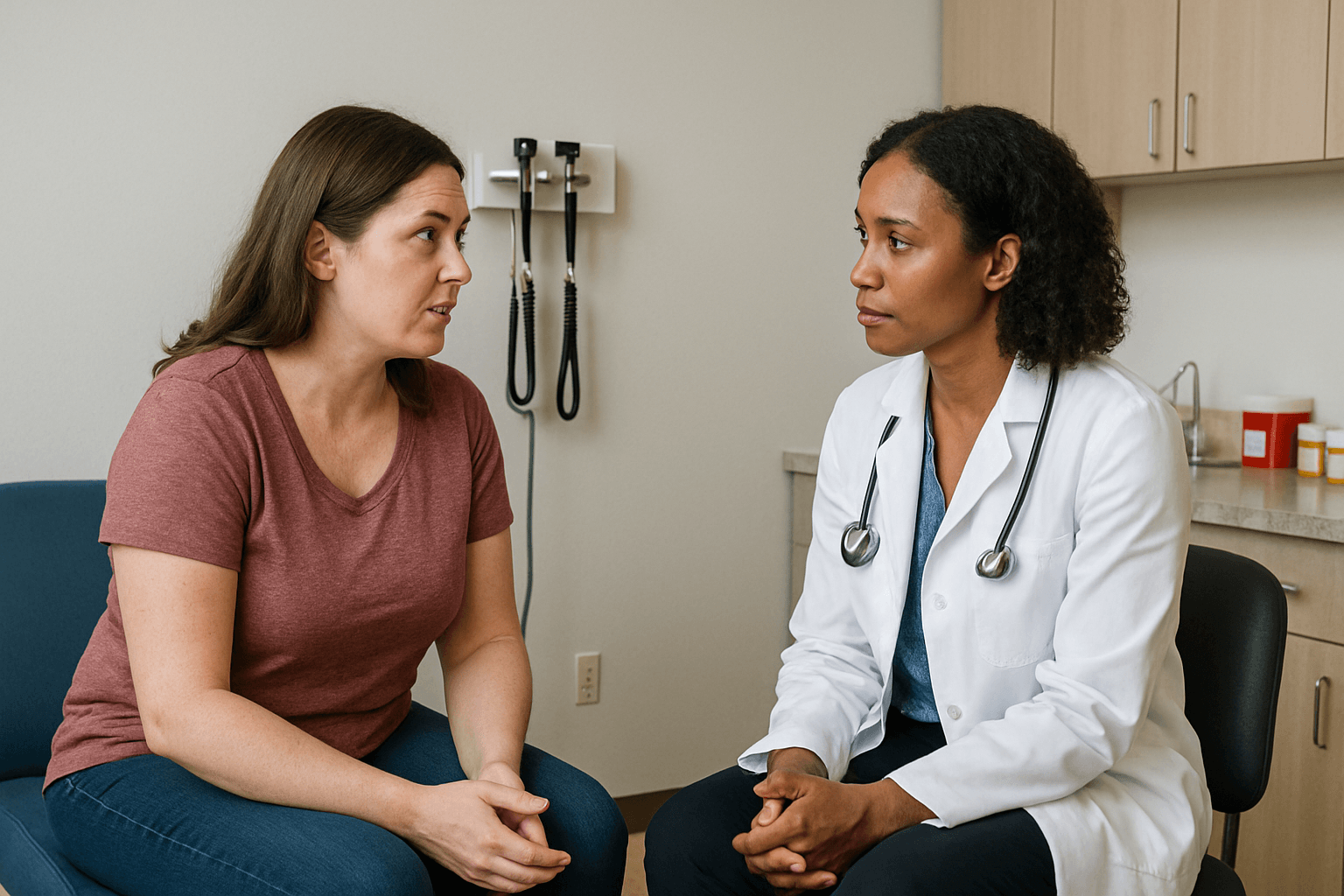
Learn 6 simple steps to ask your doctor for a GLP-1 prescription and talk confidently about safe, effective weight-loss options.
